The Gum: An Important Tissue
The gum is an essential component of the mouth: by enclosing the teeth and covering the bony structures (the alveolar bone), it provides both protection and support.
More precisely, it is the attached gingiva that supports the teeth by being attached to the alveolar bone; the gingiva also includes the free mucous membrane, which is the part that is not attached to the teeth.
During a dental examination, special care is paid to your gums, which are essential to the preservation of your teeth. Since they are particularly sensitive by nature, they are vulnerable and can easily develop various diseases and infections. By making an appointment with your dentist, you can prevent these at the source.
Here are some aspects that characterize healthy gums:
- The colour is pink and there is no redness or swelling
- The volume and firmness are adequate and allow the teeth to be well supported; the gum is completely glued to the teeth
- The root is not visible; the gum plays its role of protection of the internal parts of the tooth
- The absence of bleeding during the oral hygiene routine (toothbrush and dental floss)
The Periodontium
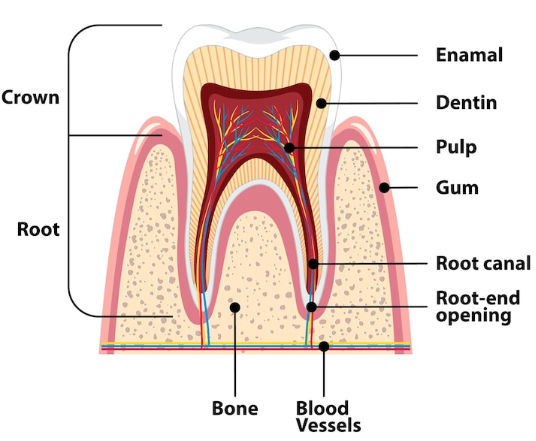
The periodontium is composed of several tissues whose function is to support and protect the tooth.
It includes the gum and its different parts (18, 19, 20, 21), a soft tissue.
The alveolar bone (23) refers to the bone structure covered by the gum; it is in this part of the jaw that the teeth take root.
The cementum (7) surrounds the dentine in the inner part of the tooth: it is a hard tissue that protects the root.
Between the cementum and the alveolar bone, the periodontal ligament (22) is a tissue composed of fibres that also surrounds the root.
Finally, a set of nerves and blood vessels are located near the tooth and are part of the periodontium.

Each of the components of the periodontium is essential to maintain and protect the teeth. Consequently, inflammation, disease or any other problem affecting the periodontal tissues can make the teeth more vulnerable. They can then be exposed (especially to bacteria), lose their stability and risk infections. Not taking care of a periodontal condition can even lead to tooth loss.
A regular visit to your dentist can detect periodontal health problems. With a thorough check-up examination, it is possible to prevent the damage that can occur when your periodontium begins to show problem(s).
Gum Disease
The gums are a particularly sensitive soft tissue and gum disease is common: according to the Canadian Dental Association, it is the main dental problem encountered by the population. Often benign at first, these diseases are easy to treat and heal: it is therefore important to detect them as soon as they occur. However, when no care is taken to maintain gum health, these diseases can develop and become more serious, frequently without any pain at first. If left untreated, this can lead to unfortunate consequences, as the disease can spread to the entire periodontium.
Early detection of disease and immediate treatment can often save you from more complex and costly procedures. It is even possible to treat the onset of disease or infection before you experience any symptoms, sparing you the discomfort and pain that might otherwise be experienced.
However, when the disease is more advanced, you risk much more serious consequences. These include chronic problems, severe pain and chewing difficulties. At an even more advanced stage, it can even lead to tooth loss.
Risk Factors
Everyone needs to take care of their gum health, but some people are more likely to develop periodontal disease. These factors may depend on your dental hygiene and habits, but also on natural and biological factors over which you have no control. Your dentist will be able to inform you about your predisposition and advise you on how to avoid developing periodontal disease. Among the most important risk factors:
- Poor dental hygiene habits
- Smoking
- A weakened immune system, whether due to stress or disease (HIV or leukemia, for example)
- Inadequately controlled diabetes
- Pregnancy or menopause, due to hormonal changes
- Medication intake that have harmful side effects on the gums
How Gum Disease Develops
The mouth naturally contains a very large number of bacteria. When you eat food, these bacteria produce acids, which mix with other particles in your mouth and with proteins in your saliva. This mixture produces a slimy substance called biofilm, which is a thin film that sticks to the tooth walls. Biofilm is normal and not dangerous, but it must be removed as soon as possible. The best way to remove this layer is to brush your teeth after each meal.
If this biofilm is not removed quickly by proper brushing, it becomes plaque. At this point, it is still possible to dislodge the debris with proper cleanings and flossing. Note that brushing removes much of the plaque, but about one third of it is only accessible through flossing. Your dentist will probably repeat it over and over, but flossing is essential for good oral health.
However, if you don’t remove plaque on a daily basis, it will mineralize and turn into tartar. It is important to note that tartar cannot be removed by brushing or flossing; it can only be removed by professional scaling.
Plaque and tartar are responsible for tooth decay and gum problems. Bacteria multiply very quickly on plaque and tartar, which are essentially food debris.
Although scaling is not normally painful, if tartar buildup under your gums leads to infection or gingivitis, it could be a rather unpleasant time to spend. You may have had painful experiences with scaling in the past. At the Centre Dentaire & D’Implantologie Boucherville, have no fear: we never let our patients experience any pain whatsoever. If our team considers that the treatment may be difficult and painful for you, we will offer you pain-relieving solutions to ensure that everything goes smoothly.

Gingivitis
Gingivitis is an inflammation of the gums and is a very common condition. This inflammation develops because of an accumulation of plaque and tartar that has not been removed.
Adults are often affected, but children and teenagers also suffer from it. Anyone can develop gingivitis at some point in their lives; however, some people may be more prone to it than others. Your dentist will be able to tell you if you have a predisposition or if you are at risk.
Here are some symptoms that may alert you to the presence of gingivitis:
- A change in the colour or appearance of the gums: they turn red and become smooth and shiny
- Swelling of the gums
- Spontaneous bleeding or bleeding when brushing or flossing
- Bad breath that persists, despite good dental hygiene
Gingivitis itself is rarely serious: not only is it rarely painful, but it does not affect the dental and periodontal structures. Pain can sometimes appear with the inflammation. However, since the gum is a sensitive periodontal tissue, it is the first stage of periodontal disease, which can develop and attack dental structures.
The good news concerning gingivitis is that it is easily curable and preventable when improvements are made to oral hygiene. This means that gingivitis is reversible and does not degenerate if treated early.
If you see signs of gingivitis, it is very important to continue brushing and flossing properly even if your gums are bleeding.
The 3 Types of Gingivitis
- Simple or chronic gingivitis: This gingivitis mainly manifests itself as swelling, redness, bleeding, and a smooth appearance of the gums; it is usually painless. It is the type of gingivitis that appears when there is an accumulation of plaque and tartar due to poor dental hygiene habits. Therefore, it is easy to prevent it by simply taking care of your teeth.
- Ulcero-necrotic gingivitis: This type of gingivitis includes the same symptoms as the first, plus pain and more bleeding. It is most commonly found in people with a weakened immune system. The bacteria are more aggressive, and can lead to consequences such as a gap between the teeth and the gum, due to gum destruction.
- Hypertrophic (hyperplastic) gingivitis: This gingivitis is usually recognized by swollen gums, which are more prominent than with other types of gingivitis; this can be problematic when cleaning. There may also be a change in the composition of the gums, which becomes more fibrous, in the case of hyperplastic gingivitis. This type of gingivitis is more related to the side effects of certain medications.

Periodontitis: A More Serious Condition
When gingivitis appears and is not treated, it spreads to the periodontium, i.e., to all the tissues that support the tooth. This is called periodontitis, an advanced stage of gum disease. This disease is much less benign than gingivitis, as it can have serious consequences. Indeed, since the periodontium supports the tooth, periodontal disease can ultimately lead to the fall of the tooth.
This is due to the fact that plaque and tartar, which are not dislodged, reach the periodontal pockets surrounding the tooth. Thus, the bacteria will gradually attack all the tissues of the periodontium, including the ligament and the alveolar bone in which the teeth are held.
The first effects of periodontitis are generally a loosening of the teeth and an abnormal mobility of these. If left untreated, they will eventually fall out or have to be removed. Again, even at this advanced stage, there may not be any pain, so it is important to remain vigilant.
Periodontitis has several causes, including a large number of bacteria present in the periodontal pockets, often linked to poor hygiene habits. Smoking is another habit that can lead to periodontitis.
It can also be caused by factors beyond the patient’s control, such as genetics, diabetes, or diseases that affect the immune system, leaving the body unable to fight the infection.
Evolution of After Gingivitis, Comes Periodontitis
The gum is one of the tissues that make up the periodontium, so when gingivitis develops, it spreads to other periodontal tissues and turns into periodontitis. Gingivitis is often painless, which means that it can progress without the patient even knowing that he or she has it.
Therefore, it is important to be attentive: regularly inspect your gums for any changes in their appearance and consult your dentist quickly if unusual signs appear. While gingivitis is easily treated and prevented, it is better not to wait for it to develop into periodontitis, which can create irreversible damage. As mentioned, periodontitis can destroy the alveolar bones and lead to irreparable tooth loss.
Fortunately, not all gingivitis develops into more severe periodontal disease, but any signs of gingivitis should still be taken seriously.

How to Prevent these Diseases
There are several simple, healthy oral habits that can help prevent the onset of gum and periodontal disease:
- Floss: Once a day, preferably at bedtime, floss before brushing your teeth. To do this, wrap the floss around your middle fingers for easier control. Flossing removes a lot of debris that a toothbrush can’t reach, so it’s essential.
Note that flossing should always be done before brushing to avoid bacteria being sprayed on the teeth you have just cleaned.
- Brush your teeth: at least twice a day, once at bedtime, brush your teeth to remove bacteria, food debris and plaque that has formed on the surface of your teeth. Ideally, brushing should be done after each meal to avoid plaque formation.
Note: While we learn how to brush our teeth at a young age, many adults forget or neglect to do it properly. Don’t hesitate to ask your dentist for advice.
- Toothpaste: If you are prone to gingivitis or periodontal disease, there are antibacterial or anti-gingivitis toothpastes specially designed to help you prevent these problems. Your dentist will be able to suggest the toothpaste best suited to your teeth.
- Quit smoking: Although it is not easy to quit smoking, smoking has many consequences on oral health and promotes the development of gum and periodontal diseases. To maintain healthy teeth, smokers benefit greatly from quitting smoking.
Visit your dentist regularly: Depending on your needs and the specific problems of your teeth, your dentist will be able to recommend an optimal frequency of visits. In general, one visit per year is necessary; you may have less frequent visits, for example every six months.
A clinical examination at this time can detect any problems or diseases at an early stage. Teeth and gums are carefully inspected, and X-rays allow the dentist to detect conditions that would not be detectable with the naked eye, so that they can be treated as soon as possible.
A cleaning and scaling are also part of these essential visits, and the team of health professionals will be able to give you personalized advice to prevent the development of dental and gum disease. Pregnant women should also have a dental check-up, ideally during the second trimester, to ensure that there are no changes or concerns about their oral health.
Gum recession: Also known as receding teeth, gum recession occurs when the gums become thinner or recede, resulting in gum loss. Recession can be mild, but when a significant amount of gum tissue is missing, it can lead to more serious consequences. Indeed, when the gums can no longer support the tooth, the latter can fall out since it no longer has a solid anchor.
There are several possible causes; often, inadequate or overly aggressive tooth brushing can lead to this loosening. It can also be a side effect of gum disease or orthodontic treatment. When recession occurs, the teeth appear increasingly longer, and this can lead to exposed tooth roots, exposed to air and bacteria. Monitoring your gums and making regular visits to the dentist are good habits to develop to prevent the onset and worsening of problems like gum recession.
